Circadian rhythm sleep disorders are conditions that happen when your internal body clock doesn't match your external environment. Your body has a master clock called the suprachiasmatic nucleus (SCN) in your brain that controls when you feel sleepy and alert. When this clock falls out of sync with the light-dark cycle around you, it creates persistent sleep problems.
There are six main types of circadian rhythm sleep disorders. Each affects sleep timing differently, but all cause similar issues: trouble sleeping at desired times and daytime fatigue. This guide covers the different types, their symptoms, and proven treatments that can help reset your internal clock.
What Are the 6 Types of Circadian Rhythm Sleep Disorders?
The six recognized types of circadian rhythm sleep disorders each affect your sleep timing in different ways. Some shift your schedule earlier or later, while others create irregular patterns or cause your clock to drift continuously. Understanding which type you might have is the first step toward effective treatment.
1. Delayed Sleep Phase Disorder (DSPD)
People with DSPD are natural "night owls." Their internal clock runs later than typical sleep schedules. They can't fall asleep until very late at night (often 2-6 AM) and struggle to wake up for morning commitments. When they do sleep, the quality is normal. The problem is timing.
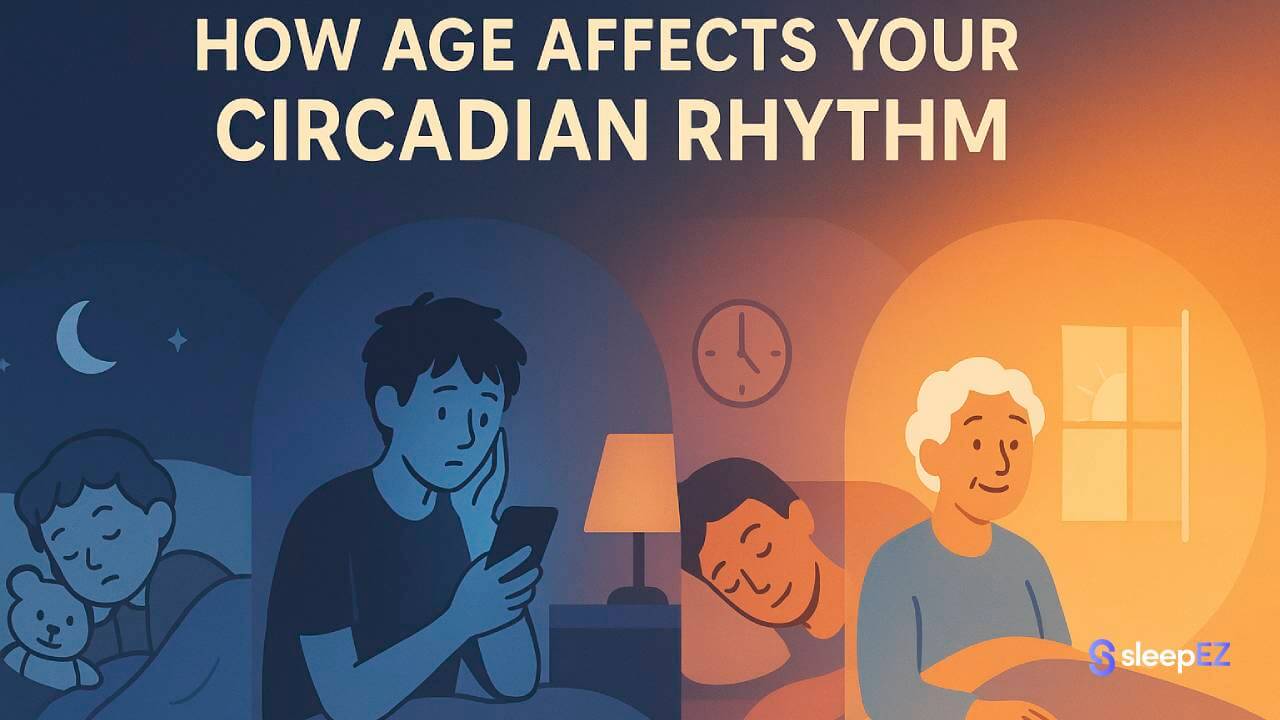
This disorder commonly appears during adolescence and affects 7-16% of teenagers, according to the National Institute of Neurological Disorders and Stroke. Many people with DSPD are mislabeled as having insomnia when the real issue is their shifted clock.
2. Advanced Sleep Phase Disorder (ASPD)
ASPD is the opposite of DSPD. These "early birds" feel extremely sleepy in the early evening (6-9 PM) and wake up very early (2-5 AM). The condition is less common than DSPD and typically affects older adults. Their sleep is normal in quality and duration, just shifted earlier than social norms.
3. Irregular Sleep-Wake Rhythm Disorder
This disorder involves a disorganized sleep pattern with no clear sleep-wake cycle. People sleep in multiple short periods throughout the day and night instead of one main sleep block. The total sleep time over 24 hours may be normal, but it's fragmented.
This condition often occurs in people with neurodegenerative diseases like Alzheimer's or after brain injuries. The SCN loses its ability to maintain a consistent rhythm.
4. Non-24-Hour Sleep-Wake Rhythm Disorder
In this disorder, the internal clock runs on a cycle longer than 24 hours (usually 25 hours). Each day, sleep and wake times drift later and later. Someone might sleep at midnight one week, then 3 AM the next week, then 6 AM after that.
This condition primarily affects people who are totally blind, as reported by Cleveland Clinic. Without light cues to reset the clock daily, it free-runs on its natural longer cycle. Some sighted people can also develop this rare condition.
5. Shift Work Sleep Disorder
This disorder affects people whose work schedules conflict with their natural sleep-wake cycle. Night shift workers, rotating shift workers, and early morning workers often develop this condition. Their work requires them to be awake when their body expects to sleep.
The Sleep Foundation notes that 10-40% of shift workers experience this disorder. Symptoms include insomnia when trying to sleep during the day and excessive sleepiness during night shifts.
6. Jet Lag Disorder
Jet lag happens when you travel quickly across multiple time zones. Your internal clock stays synced to your home time zone while your environment shifts. This creates temporary misalignment.
The more time zones you cross, the worse the symptoms. Flying east (which shortens your day) typically causes worse jet lag than flying west. Most people naturally adjust within a few days.
Symptoms of Circadian Rhythm Sleep Disorders
While each type of circadian rhythm disorder has unique characteristics, they all share similar symptoms. These symptoms occur because your body is trying to sleep or stay awake at times that don't match your internal clock. The result is poor sleep quality and daytime impairment that affects work, school, and daily activities.
Common symptoms include:
- Difficulty falling asleep at the desired time (insomnia)
- Difficulty staying asleep through the night
- Excessive daytime sleepiness (EDS)
- Waking up too early and being unable to fall back asleep
- Non-restorative sleep (waking up feeling tired)
- Impaired concentration and memory problems
- Decreased alertness and performance
- Mood changes and irritability
The severity depends on how far your internal clock differs from your required schedule. Someone with DSPD working a 9-5 job suffers more than someone with a flexible schedule.
What Causes These Disorders?
The root cause is a mismatch between your internal SCN and external time cues (mainly light and dark). Several factors contribute:
Genetics: Some people inherit genes that affect clock timing. Research from the National Institutes of Health shows specific gene mutations can cause DSPD and ASPD to run in families.
Age: Circadian rhythms change naturally with age. Teenagers' clocks shift later (making DSPD more common), while older adults' clocks shift earlier (making ASPD more common).
Light exposure: Modern artificial light at night can confuse the SCN. Blue light from screens is particularly disruptive. Insufficient bright light during the day also weakens circadian signals.
Neurological conditions: Brain injuries, dementia, and developmental disabilities can damage the SCN or its connections, causing irregular sleep-wake patterns.
Work and lifestyle: Shift work and frequent travel across time zones force the body to operate against its natural rhythm.
How Are Circadian Rhythm Disorders Diagnosed?
Diagnosis starts with consulting a doctor or sleep specialist. They'll review your medical history and sleep complaints. Several tools help confirm a circadian rhythm disorder:
Sleep diary or sleep log: You track your sleep and wake times for at least two weeks. This reveals patterns in your natural sleep timing. The diary should note when you go to bed, when you fall asleep, when you wake up, and how you feel.
Actigraphy: You wear a device on your wrist (similar to a fitness tracker) that monitors movement and light exposure. It records your sleep-wake patterns over one to two weeks. This objective data confirms what your sleep diary shows.
Sleep studies: In some cases, an overnight sleep study (polysomnography) rules out other sleep disorders like sleep apnea. However, this isn't always necessary for circadian rhythm disorders.
Dim light melatonin onset (DLMO) testing: This specialized test measures when your body starts producing melatonin in the evening. It's the most accurate way to assess your circadian phase but is mainly used in research settings.
Treatment for Circadian Rhythm Sleep Disorders
Treatment aims to realign your internal clock with your desired schedule. Different approaches work for different disorders.
Bright Light Therapy (Phototherapy)
This treatment uses a specialized light box that produces bright light (typically 10,000 lux). You sit near the light box at specific times to shift your circadian rhythm.
For DSPD, you use bright light in the morning to shift your clock earlier. For ASPD, you use bright light in the evening to shift your clock later. Treatment sessions usually last 30-60 minutes.
The National Center for Biotechnology Information reports that bright light therapy is one of the most effective treatments for circadian disorders. Results appear within one to two weeks, but continued use maintains the shift.
Melatonin Supplements
Melatonin is a hormone your body produces naturally to signal sleep time. Taking melatonin supplements at strategic times can shift your circadian phase.
For DSPD, you take low-dose melatonin (0.5-3 mg) in the early evening to advance your clock. For ASPD, you take it in the early morning to delay your clock. Timing matters more than dose.
The Sleep Foundation notes that melatonin works best when combined with light therapy. It's generally safe for short-term use, but you should consult a doctor about proper timing and dosage.
Chronotherapy
This structured approach involves progressively shifting your sleep schedule in the direction your body naturally wants to go. For DSPD, you might delay your bedtime by 2-3 hours each day until you circle around to your desired schedule.
This treatment requires several weeks and strict adherence. You must maintain the new schedule once achieved. Chronotherapy works well for motivated individuals but can be difficult to complete while working or going to school.
Lifestyle Adjustments & Good Sleep Hygiene
Creating the right sleep environment and maintaining consistent habits supports your circadian rhythm:
- Keep a consistent sleep schedule, even on weekends
- Get bright light exposure in the morning
- Avoid bright light and screens 2-3 hours before bedtime
- Keep your bedroom dark, quiet, and cool
- Avoid caffeine after early afternoon
- Avoid alcohol close to bedtime
- Exercise regularly, but not close to bedtime
Practicing good sleep hygiene is a foundational step in managing these disorders. This involves creating an ideal sleep environment, which can be difficult for those with shift work or DSPD. Using tools to take control of your environment can help significantly.
A bluetooth sleep mask blocks unwanted light and lets you listen to relaxing audio. Silicone earplugs and sound machines mask disruptive noise effectively.
Frequently Asked Questions
Q: What is the difference between insomnia and a circadian rhythm disorder?
A: Insomnia is difficulty falling or staying asleep even when you have the right opportunity to sleep. Circadian rhythm disorders are timing problems. You can sleep well, but only at the wrong times. Someone with DSPD sleeps fine from 3 AM to 11 AM. Someone with insomnia can't sleep well even in ideal conditions at any time.
Q: Can circadian rhythm disorders be cured?
A: It depends on the type. Jet lag is temporary and resolves on its own within days. Shift work disorder improves if you stop working shifts. However, conditions like DSPD and ASPD are often lifelong. They can't be cured, but they can be managed effectively with ongoing treatment. Many people learn to work with their natural rhythm by choosing flexible schedules or remote work.
Conclusion
Circadian rhythm sleep disorders affect when you sleep rather than whether you can sleep. The six main types (DSPD, ASPD, irregular sleep-wake rhythm, non-24-hour sleep-wake rhythm, shift work disorder, and jet lag) each create different timing problems but share common symptoms like daytime fatigue and difficulty sleeping at desired times.
These disorders stem from a mismatch between your internal clock and your environment. Bright light therapy, melatonin supplements, chronotherapy, and lifestyle changes can realign your rhythm. Some conditions are temporary while others require long-term management.
If you experience persistent problems with sleep timing that affect your daily life, consult a doctor or sleep specialist. Proper diagnosis and treatment can significantly improve your sleep quality and daytime functioning.

Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.